U. Pignatelli, L. Gentile, G.P. D’Addazio, P. Gamba, G. Licursi, U. Moz
ENT Unit Poliambulanza Foundation Brescia Italy
ABSTRACT
Introduction: ChroWe related about a case of Lemierre’s disease, treated at the ENT Department of Poliambulanza Hospital Foundation in Brescia (Italy) . Lemierre’s is a rare disease, characterized by a history of recent oropharyngeal infection , clinical or radiological evidence of internal jugular vein thrombosis, and isolation of anaerobic pathogens, mainly Fusobacterium necrosphorium. In our case there is a localization in right ear and lung. We discussed about diagnosis, treatment and need of multidisciplinary team approach. Key Words: Lemierre’ disease – ENT localization – Diagnosis and treatment.
CASE REPORT
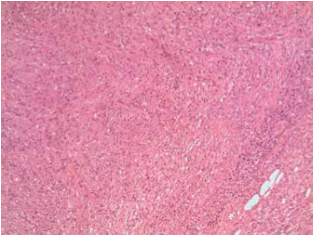
A young Albanian man of 23 years old arrived to the Emergency Department of Poliambulanza Hospital Foundation complaining for headhache and right ear pain. Recent medical history consinstent with a lung lobectomy for abscess about 1 month before; past medical history of right chronic othitis from childhood . ENT valutation: chronic othitis with othorrea and redness of the retroauricular skin, pain at soft digital pression, persistent headhache. Suspecting for Lemierre disease a CT scan was performed with evidence of:“ …big deishence of posterior wall of right mastoid near sigmoid sulcus …. the material is like brain-fluid. The ear cavity is full of material like infiammatory tissue and encase the ossicular chain ;thrombosis of ipsilateral sigmoid lateral vein” (Fig. 2). The auditory exame was : hypoacusis of all frequencies with bone gap middle down. Surgical andmedical evaluation decided for a multisciplinary approach that was: antibiotic therapy with Metronidazole 500 mg every 8 hours and Meropenem 1 gr every 8 hours and surgery: after surgery started therapy with subcutaneos low-molecular-weight heparin (LMWH). We operated on the patient in emergency state : we perfomed open timpanoplasty with mastoidectomy finding a big amount of pathologic secretions and colesteatoma in mastoid cavity with thrombosis of lateral sinus: we cleared all even the middle ear cavity with preservation of ossicular chain ( malleus and staple: incus had a large mutilation and was removed). The post surgery course was good without complication and the patient was discharged after 5 days. The antimicrobial culture isolate: Fusobacterium Necrosporium. The pathologic report was:
1) From mastoid and middle ear cavity: cheratinic lamellar material
2) From middle ear cavity about sentinel polip: infiammtory polip
3) From tissue near right lateral sinus: granulation tissue
After 1 month the cavity was good without disease and there was no headache. The patient went back home (Albania). At the check phone call he was fine : we recommended him to do ENT periodic visit.
DISCUSSION
In 1936 Andre Lemierre 1 pubblished a description of 20 cases in the Lancet that involved the costellation of sepsis, metastatic pulmonary lesions and, most commonly ,the isolation of Bacillus Fundiliformis now known as Fusobacterium necrophorum3 6. The male to female ratio is 1:1,2 and the ages ranged from 2 months to 78 years .Most cases present in 2nd decade of life (51%),followed by the 3rd decade (20%),and then the 1st decade (8%). The main sources of infection are tonsil, pharynx, and chest followed by larynx and middle ear . The most common first clinical presentation is a sore throat ,followed by neck mass and neck pain. The main 12offending microorganisms are F.necrosphorum(57%), F.species (30%) and F. Nucleatum (3%) ,followed by anaerobic streptococci and other miscellaneous Gram-negative anaerobes(10%). Mortality is encountered in 5%. The first line investigation is chest X ray but the the most commonly requested scan is CT scan of neck/chest, ultrasound, MRI. The treatment modalities are antimicrobical 10 , anticoagulant, and surgical treatment or a combination of the above. The antimicrobial 11 treatment is metronidazole, ampicillina/sulbactam, imipenem, meropenem, betalactam/betalactactamase inhibitors combinations (eg, piperacillin/tazobactam): the duration of treatment ranging between 3 and 6 weeks: relapses have been documented when treatment was given for less than 2 weeks The anticoagulation1 is administrated in 30% of the patients and expecially in cases with internal vein jugular thrombosis, brain complications or septic thrombotic pulmonary emboli( at fisrt LMHV subcutaneous enoxaparin 1mg/kg twice daily with conversion to warfarin achieved a targed international normalization ratio between 2 and 3 for a therapeutic duration of 3 months) The surgical treatment is focused to remove septic foci 8( pulmonary,jugular vein thrombosis, abscess of brain or mastoid and middle ear cavity). Even in our case we treated the patient with a combination of metronidazole and meropenem,open timpanoplasty with mastoidectomy and subcutaneous low weight enoxaparin. In conclusion for a successfull resolution of Lemierre’s disease we need of multisciplinary approache.
REFERENCES
1) Karkos PD, Asrani S, Karkos CD, Leong SC, Theochari EG, Alexopoulou TD, Assimakopoulos AD. Lemierre Syndrome: A Systematic Review. Laringoscope 2009; 119: 1552-1559
2) Wright WF ,Shiner CN, Ribes JA. Lemierre syndrome. South. Med. J. 2012; 105(5): 283-8.
3) Kuppalli K, Livorsi D, Talati NJ, Osborn M.Lemierre’s syndrome due to Fusobacterium necrophorum Lancet Infectious diseases 2012;12(10): 808-815.
4) Brown LM, Wallwork B. Lemierre’s – the sinister sore throat. J. Laryngolol Otol 2007; 121: 692-694.
5) Ockrim J, Kettlewell S, Gray GR. Lemierre’s syndrome. J.R. Soc. Med. 2000; 93:480-481.
6) Giridharan W, De S, Osman Ez,et al. Complicated otitis media caused by Fusobacterium necrophorum. J. Laryngol. Otol. 2004; 118:50-53.
7) Bentham JR, Pollard Aj, Milford CA, et al. Cerebral infarct and meningitis secondary to Lemierre’s syndrome. Pediatr Neurol. 2004;30: 281-283
8) Shaham D, Sklair-Levy M, Weinberger G, Gomri J.M. Lemierre’s syndrome presenting as multiple lung abscesses. Clin. Imaging 2000;24:197-199.
9) Dool H., Soetekouw R, van Zanten M, Grooters E. Lemierre’s syndrome: three cases and a review. Eur arch Othorynolaringol 2005; 262: 651-654.
10) Seo YT, Kim MJ, Kim JH, et al. Lemierre syndrome: a case of postanginal sepsis. Korean J Intern Med 2007; 22:211-214.
11) Maramattom VB, Wijdicks EF. Bilateral internal jugular vein thrombosis: a benign presentation of Lemierre’s syndrome? Cerebrovasc. Dis. 205;19: 139-140.
12) Moore BA, Dekle C, Wekhaven J. Bilateral Lemierre’s syndrome: a case report and literature review. Ear Nose Throat J 2002; 81: 234-242.
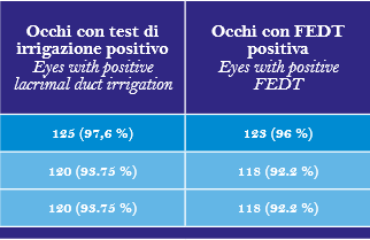
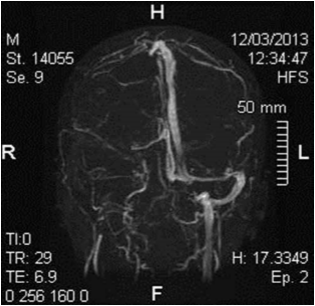 Fig. 1
Fig. 1
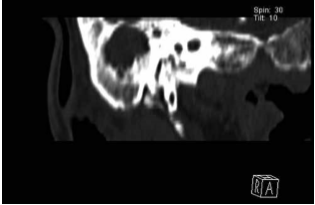 Fig. 2
Fig. 2