O. Marotta, F. Catapano, V. Marotta
UOC di Otorinolaringoiatria, Azienda Ospedaliera di Rilievo Nazionale e di Alta Specializzazione di Caserta
ABSTRACT
Klippel-Trenaunay syndrome (KTS) is a rare congenital disorder characterized by capillary malformations (port-wine stains or flat haemangiomas), soft tissue and bone hypertrophy, large varicose veins. Intracranial vascular malformations are very rare. The Authors report a case of a 4 year old girl with KTS, suffering from anacusis in the left ear and severe sensorineural hearing loss in the right ear, who underwent cochlear implantation; in our case angiomatous formations were located inside the temporal bone, one of these adherent to the vertical portion of the facial nerve.
INTRODUCTION
In 1900 Maurice Klippel and Paul Trenaunay were the first to describe a rare angio-osteoipertrofica syndrome characterized by symptom triad: capillary malformations (port-wine stains or flat hemangiomas), soft tissue and bone hypertrophy, large varicose veins (1, 2). It typically affects one lower limb, rarely more limbs, the trunk, the face or the whole body. Cases of intracranial angioma associated with KTS are very rare. Klippel-Trenaunay-Weber syndrome or Parkes-Weber syndrome is accepted as a separate entity consisting of the triad of Klippel-Trenaunay syndrome accompanied by a clinically apparent arteriovenous fistula (3). Intracranial angioma associated with KTS are extremely uncommon (4, 5, 6). The incidence is low (1/27500 births). The etiology is unknown. The disease is congenital and is due to a dysfunction of angiogenesis and vasculogenesis mechanisms of the affected sites(7). Few cases of KTS associated with hearing loss are reported in literature. In a report of Suver (8) mentions two cases: the first with sensorineural hearing loss, and the second with mixed hearing loss in a teenager with arteriovenous fistulas causing an overgrowth of bone that extended from the cochlea into the cavity of middle ear. In both cases, the typical malformation of KTS concerned the face; for this reason, the Author suggested to perform an audiological evaluation in patients with KTS interesting head.
CLINICAL CASE
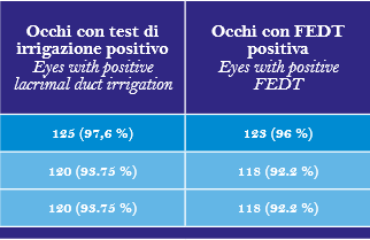
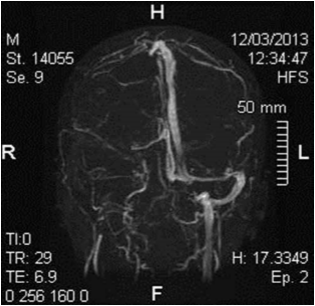
C. G. of 4 years presented to our observation for hearing loss with language delay. The parents reported that was diagnosed a KTS in the neonatal age and the audiological evaluation detected bilateral deafness, so C.G. underwent bilateral prosthesis at the age of five months and started speech therapy rehabilitation. At three years aged underwent adenoidectomy and bilateral transtympanic drainage. Despite speech therapy the patient had a noticeable language delay. For this reason she presented to our observation and we decided to perform an evaluation for cochlear implant. At physical examination, the patient had a voluminous angioma on the face and ear, neck and left shoulder; bilateral blue sclera (fig. 1 and 2). At orofaringoscopy was evident tonsillar asymmetry with the left tonsil more voluminous than the right. The tympanic membranes were intact with hyperemia of the left. Like all patients scheduled for cochlear implantation in our department, it was applied a preoperative protocol that determines the candidacy for a cochlear implant. It includes: interview, medical history and ENT examination, audiological evaluation, speech therapy evaluation, psychological evaluation, neurological – neurosurgery evaluation, neuropsychiatric evaluation, laboratory tests, cardiological evaluation, chest xray, high-resolution CT scanning of the temporal bone, brain M. R. I., anesthetic visit. The audiological evaluation revealed left anacusis and severe-profound sensorineural hearing loss on the right (fig. 3). The auditory brainstem response (ABR) highlighted the absence of significant waves in left ear; the fifth wave was present up to 90dB in right ear (Fig. 4). The speech therapy evaluation detected a language delay. Computed tomography (CT) bilaterally showed a normal cochlea and likely presence of inflammatory tissue in left mastoid (fig. 5). The MRI highlighted a hemihypertrophy of brain tissue, in particular the white matter, combined to normal morphology of the labyrinthine structures (Fig. 6).
SURGERY
The authors decided to perform cochlear implant surgery on the left ear. The preoperative anesthesia evaluation was very accurate to avoiding hemodynamic complications. The patient was evaluated ASA II. After incision behind the ear, a mastoidectomy was made. The presence of reddish gelatinous tissue that almost totally occupied the mastoid cells was highlighted. It extended in the antrum and occluded epytimpanum partially englobing the ossicular chain. While executing posterior tympanotomy, a great angiomatous formation was found that enveloped a piece of the vertical portion of the facial nerve long 5 mm (Fig. 7). Bipolar coagulation was used to cauterize and remove the angiomatous formation, taking care to preserve the nerve; so it was possible to complete the posterior tympanotomy (Fig. 8). Once the middle ear space was exposed, a anterior-inferior to the round window cochleostomy was made and the implant electrodes (ME, multi -electrodes) was inserted. The receiver/ stimulator (RS) was then placed. The neural response telemetry and stapedial reflex, used to assess CI, gave a positive result. The postoperative course was regular. The first postoperative day was performed xray, modified Stenvers view, to demonstrate the correct ME placement (fig. 9). During second postoperative day the patient was discharged. The CI was activated after one month. Subsequently C.G. undewent periodic controls and speech therapy.
DISCUSSION
KTS is a rarely associated with hearing disorders (1, 2, 8). The presence of obvious head and neck involvement, like in this case with extensive cutaneous angiomatosis and macrocrania, always requires conducting hearing screening (8). An accurate neuroradiological study is necessary to perform cochlear implantation in a patient with KTS. Although the neurovascular anomalies are rare in KTS, it could avoid serious complications related to the presence of cerebral arteriovenous malformations (4, 5, 6). The role of CT and MRI is crucial to highlight any vascular malformations affecting petrous bone. MRI with Gadolinium should be performed (), which, however, was not done in our case. The MRI demonstrated clear asymmetry of the cerebral hemispheres, finding described in literature (9, 10), resulting an increased thickness of the white matter ipsilateral to angiomatous formations. The prevalence of cerebral hemihypertrophy, in the series of 11 patients with KTS of the study, was 18%; no patient had an intracranial vascular malformation (9). The mastoid angiomatous formation did not prevent the correct execution of the operation. The formation was removed preserving the facial nerve, and six months after surgery CI works properly with considerable improvement of language.
REFERENCES
1. Klipple M, Trenaunay P. Du naevus variquex osteohypertrophique. Arch Gen Med. 1900;3:641–72
2. Cohen, M. M. (2000), Klippel-Trenaunay syndrome. Am. J. Med. Genet., 93: 171–175.
3. Lamar L. M., Farber G. A., O” Quinn S. E. Klippel-Trenaunay-Weber syndrome. Arch. Dermatol.1965;91:58–58.
4. Sadiq MF, Shuaib W. Klippel-Trenaunay syndrome with intracranial arteriovenous malformation: a rare presentation. Case Rep Radiol. 2014;2014:20216
5. Makiyama Y, Nishimoto H, Fukaya C, Tsubokawa. Massive intracerebral hematoma in a child with Klippel-Trenaunay syndrome. Surg Neurol. 1994 Nov;42(5):392-5; discussion 395-6
6. Fierek O, Laskawi R, Kunze E. Large intraosseous hemangioma of the temporal bone in a child. Ann Otol Rhinol Laryngol. 2004 May;113(5):394-8
7. Oduber CE1, van der Horst CM, Hennekam RC. KlippelTrenaunay syndrome: diagnostic criteria and hypothesis on etiology. Ann Plast Surg. 2008 Feb;60(2):217-23
8. Suver DW1, Perkins J, Manning SC. Klippel-TrenaunayWeber syndrome with labyrinthine bony overgrowth and mixed hearing loss, a case report. Int J Pediatr Otorhinolaryngol. 2004 Aug;68(8):1075-9.
9. Torregrosa A, Martí-Bonmatí L, V Higueras, Poyatos C, Sanchís a. Klippel-Trenaunay syndrome: frequency of cerebral and cerebellar hemihypertrophy on MRI. Neuroradiology. 2000 Jun; 42 (6): 420-3.
10. Hossein Esmailzadeh, Azita Tavassoli, Younes Jahangiri N, Nasibeh Vatankhah, Klippel-Trenaunay-Weber Syndrome with Hemimegalencephaly; Report of a Pediatric Case Iran J Pediatr. 2012 Mar; 22(1): 147–151.
 Fig. 1
Fig. 1
 Fig. 2
Fig. 2
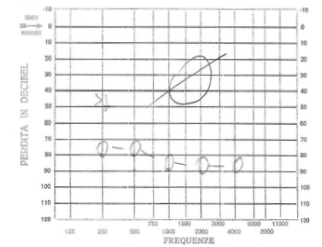 Fig. 3
Fig. 3
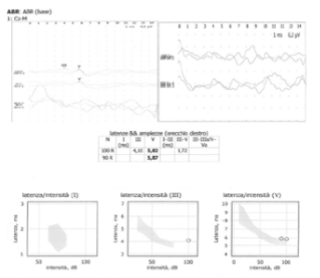 Fig. 4
Fig. 4
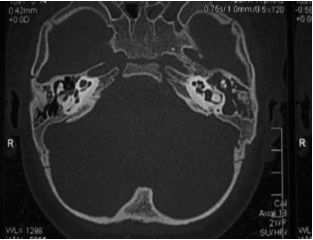 Fig. 5
Fig. 5
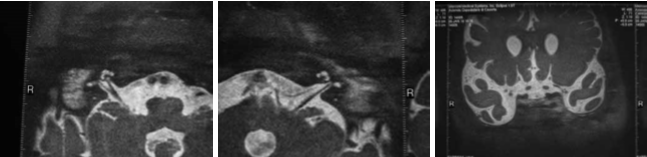 Fig. 6
Fig. 6
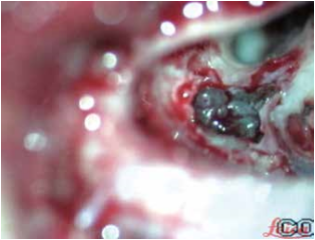 Fig. 7
Fig. 7
 Fig. 8
Fig. 8
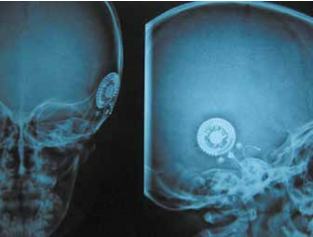 Fig. 9
Fig. 9